MRI combines strong magnetic fields and radio waves to get cross sectional images of a human body. It has the advantages of non-exposure to radiation unlike CT and it obtains different contrast enhancement levels of images. MRI uses nuclear magnetic resonance parameters, such as T1 and T2, to create images which distinguish each organ/lesion from others and make a characteristic lesion visible. Any cross section can be represented, which shows the relationship between the lesion and normal tissue surrounding it.
Two 1.5 Tesla and three 3 Tesla superconducting scanners are being used for diagnostic imaging at Hokkaido University Hospital. The 3 T scanners image a whole body, from the head to the chest, abdomen, pelvis and joint, and creates contrast-enhanced high-resolution images. The scanners respond to different imaging methods or image qualities and will be chosen depending on the patient and the position to be imaged.
3 T device (3 scanners)
1.5 T device (2 scanners)
Typical clinical examples using MRI on different organs
Central Nervous System
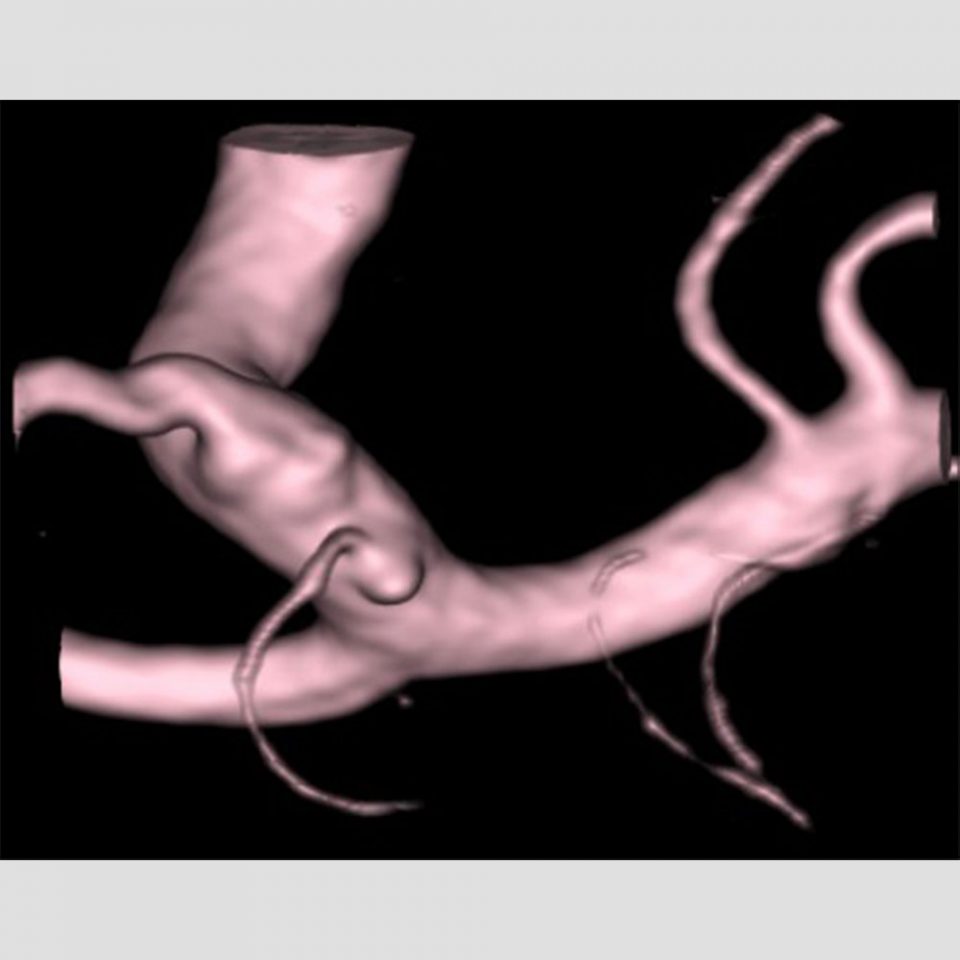
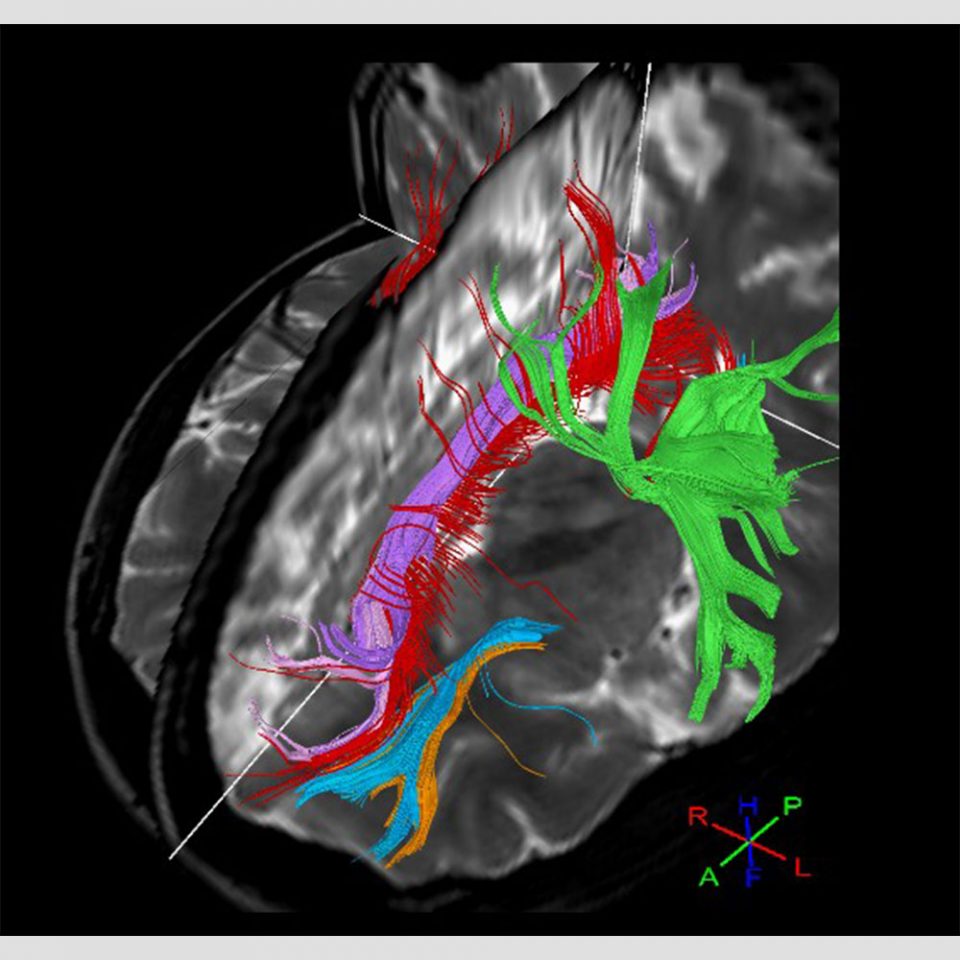
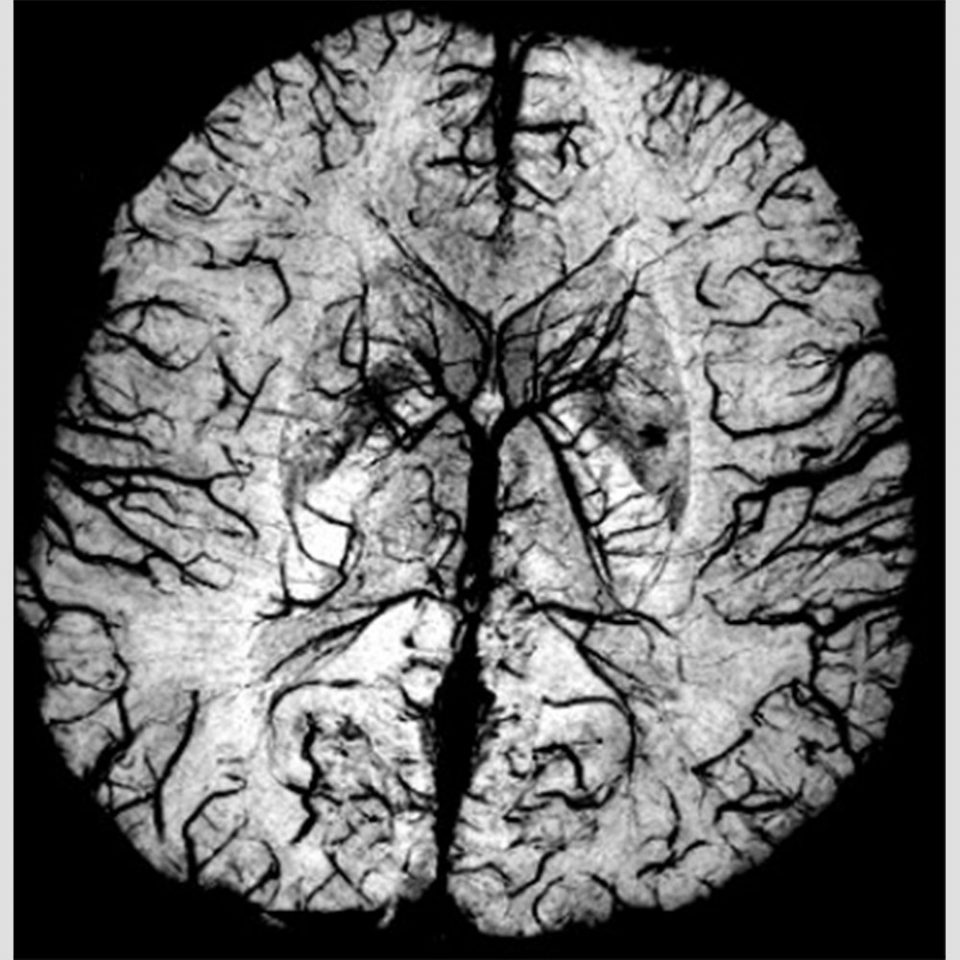
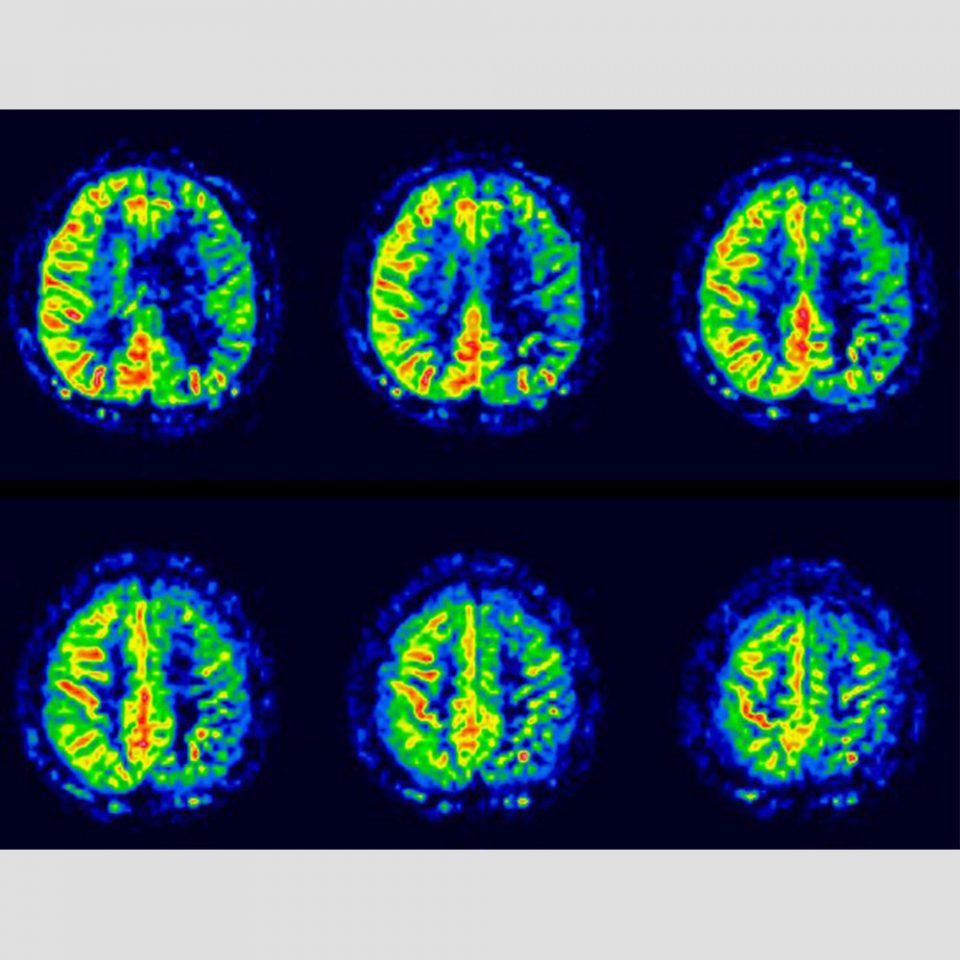
The 3 T scanners with high resolution are widely used in MR angiography and diagnosis of a small aneurysm, synthesis of brain surface anatomy and MR venography (Figure 1), 3D imaging and detection of a small metastatic brain tumor and representation of thin/narrow anatomy and cranial nerves. Special imaging methods include diffusion tensor imaging (DTI), diffusion kurtosis imaging, susceptibility weighted imaging (SWI), quantitative susceptibility mapping (QSM), arterial spin labelling (ASL), 4D flow MR angiography (4D-MRA), perfusion imaging and MR spectroscopy (MRS). DTI represents nerve tracts (tractography) to prepare for operation of a brain tumor (Figure 2). SWI and QSM represent traumatic microbleeds and normal veins most accurately. Recently, MRI is being used to study cognitive impairment. ASL and 4D-MRA allows minimally invasive cerebral perfusion scan without using contrast agent (Figure 3). MRS is a minimally invasive method to detect cerebral components and is applied to diagnose a tumor or metabolic disease (Figure 4).
Body Trunk
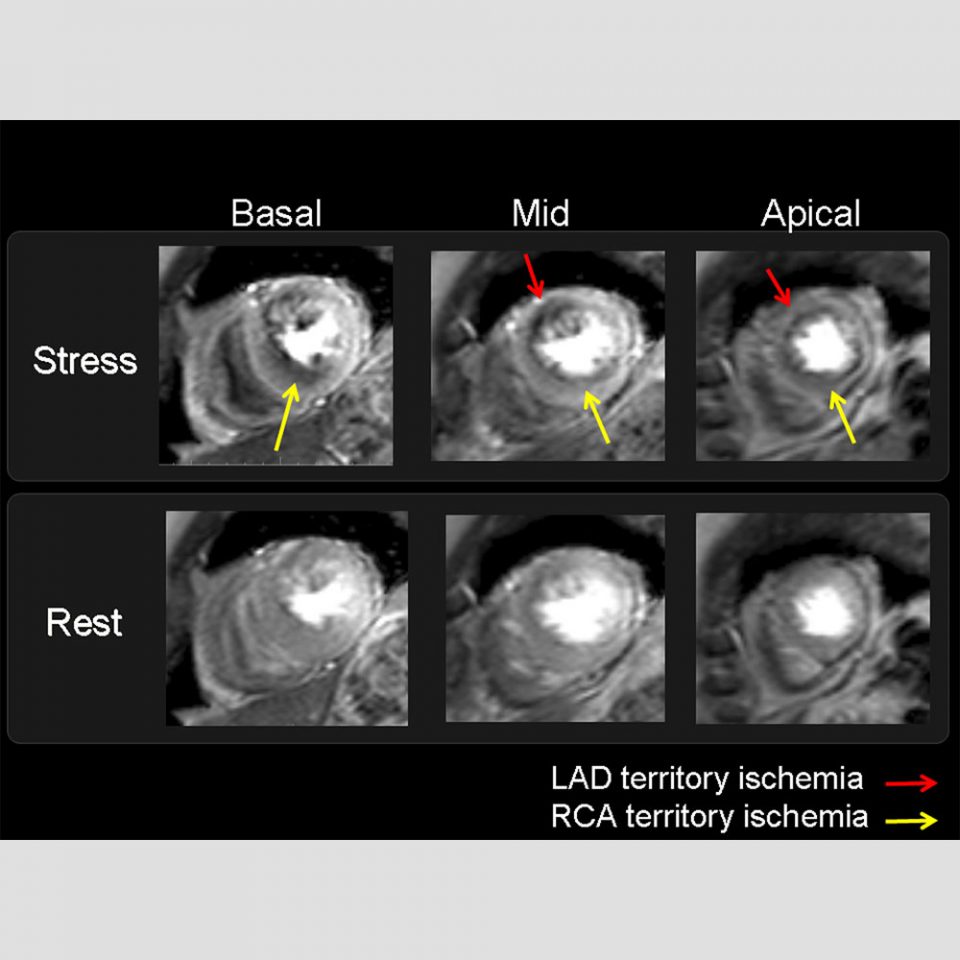
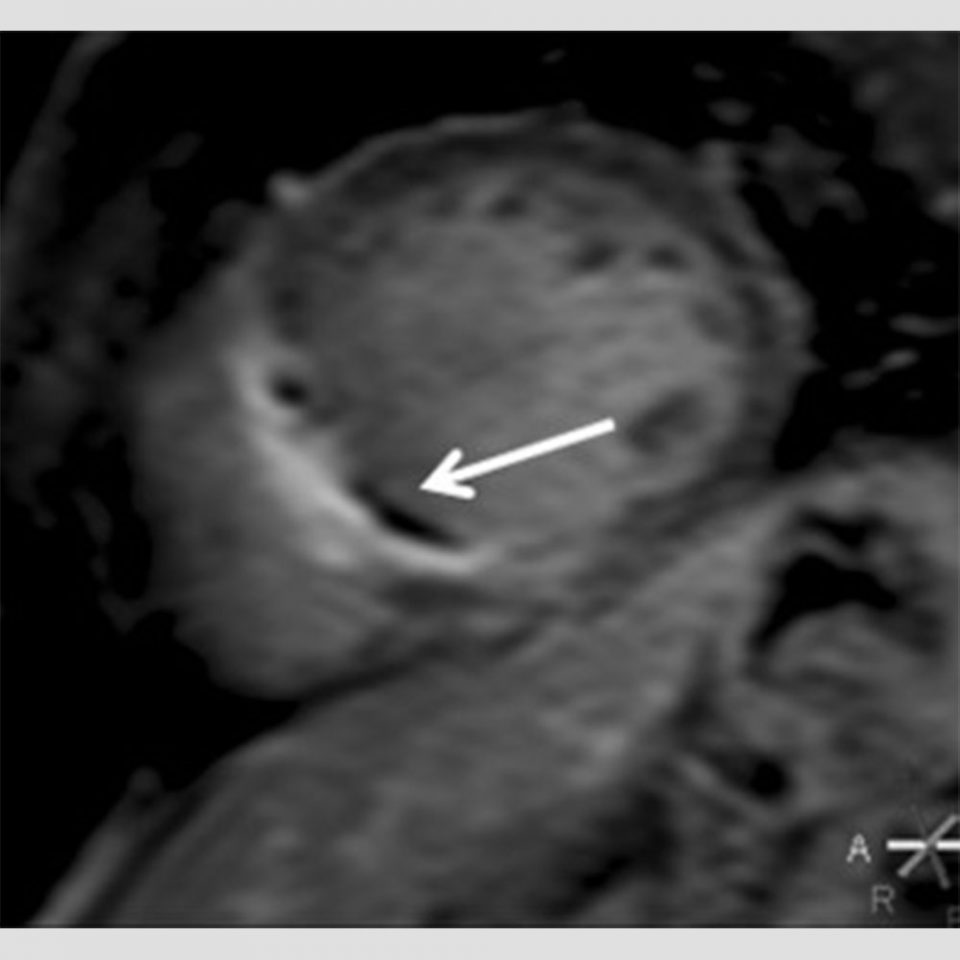
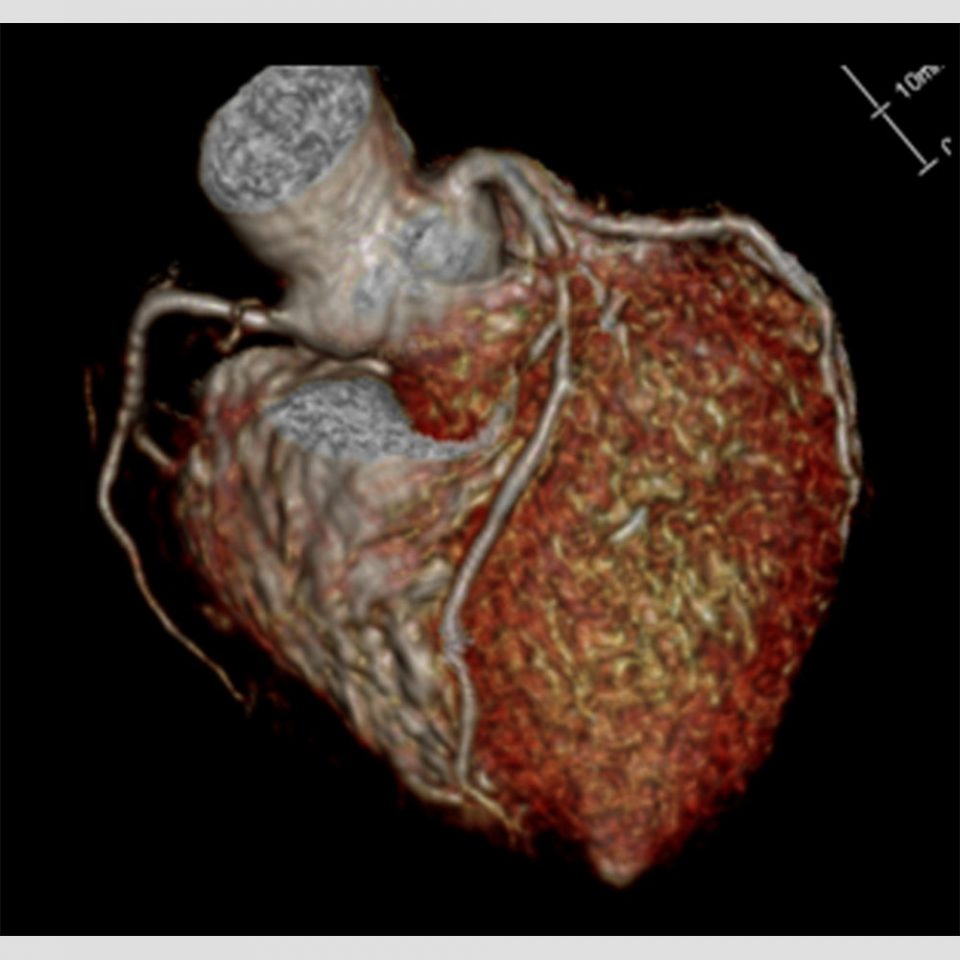
Cardiac MRI: Particularly notable MRI use is made in severe triple-vessel disease, where high-resolution contrast-enhanced perfusion MRI detects ischemic heart diseases (Figure 1). Delayed contrast-enhanced MRI and T1 mapping evaluate myocardial viability (Figure 2) and identifies cardiomyopathy types. Coronary MR angiography without contrast is also available (Figure 3).
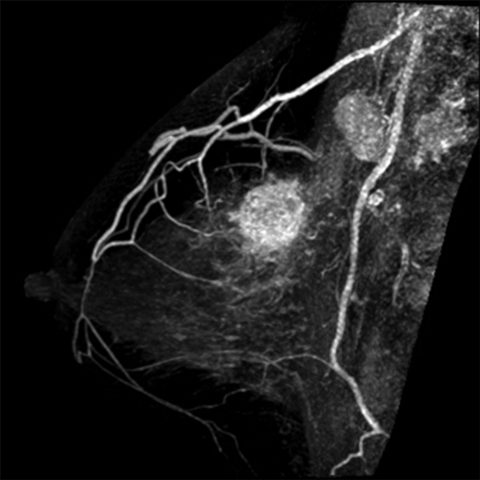
Breast MRI: The 3 T scanners allow dynamic contrast-enhanced imaging for evaluating tumor blood flow and high-resolution imaging for detailed evaluation of tumor morphology to determine the spread of cancer prior to operation. Three dimensional images, which visualize the position/spread of breast cancer, help doctors make a treatment plan (Figure 4). They are also used to check for the effect of preoperative chemotherapy or hormone therapy.
Pelvic MRI: It is widely applied in clinical settings to diagnose many gynecologic diseases, including uterine fibroid (Figure 5), uterine adenomyosis, endometriosis and ovarian tumor. It is also used to evaluate the stage, therapeutic effect, recurrence, etc. of gynecologic cancer, including endometrial/cervical/ovarian cancer. The latest imaging technology and high-definition imaging enable detection of a microscopic lesion and accurate determination of the cancer stage prior to treatment. Fetal malformation and placenta are assessed in obstetrics.

Abdominal MRI: MRI is effective in diagnosing stomach diseases, such as hepatopancreatic and gastroenterological diseases. For example, MR Cholangiopancreatography (MRCP) represents the gallbladder, biliary duct and pancreatic duct clearly. It is particularly useful in imaging stones in the gallbladder or biliary duct, which cannot be detected by CT. Hepatic MRI (EOB-MRI) using hepatocyte-specific gadolinium agent evaluates contrast-enhanced blood flow kinetics and hepatic cell functions at one time and is most effective in diagnosing metastatic hepatic tumor and hepatic cell carcinoma.
MRI of bone and soft tissue: Contrast resolution (obvious signal differences between organs) makes MRI stand at advantage over CT or a regular X-ray in representing the elements comprising joints, such as tendon, muscle, ligament and meniscus. It is also useful to check for damages, such as edematous changes and ruptures, and is widely applied to diagnose injury or degenerative disease.
Various imaging methods can be combined to diagnose neoplastic diseases in bone and soft tissue. The spread of the diseases and their characteristics are useful information for clinical services.